Ian Jackson of the Bromley by Bow Health Partnership was the guest speaker at the first Glasgow Centre for Population Health (GCPH) seminar series of the year.
The Bromley by Bow Health Partnership (BBBHP) is a collaboration between three health centres and other non-primary care partners in the Tower Hamlets area of London. The aim of the partnership – and the new primary care delivery model which comes with it – is to transform the relationship between the public and primary health care. This means considering the wider determinants of health when the partners plan and deliver care, rather than treating healthcare in a purely biomedical way.
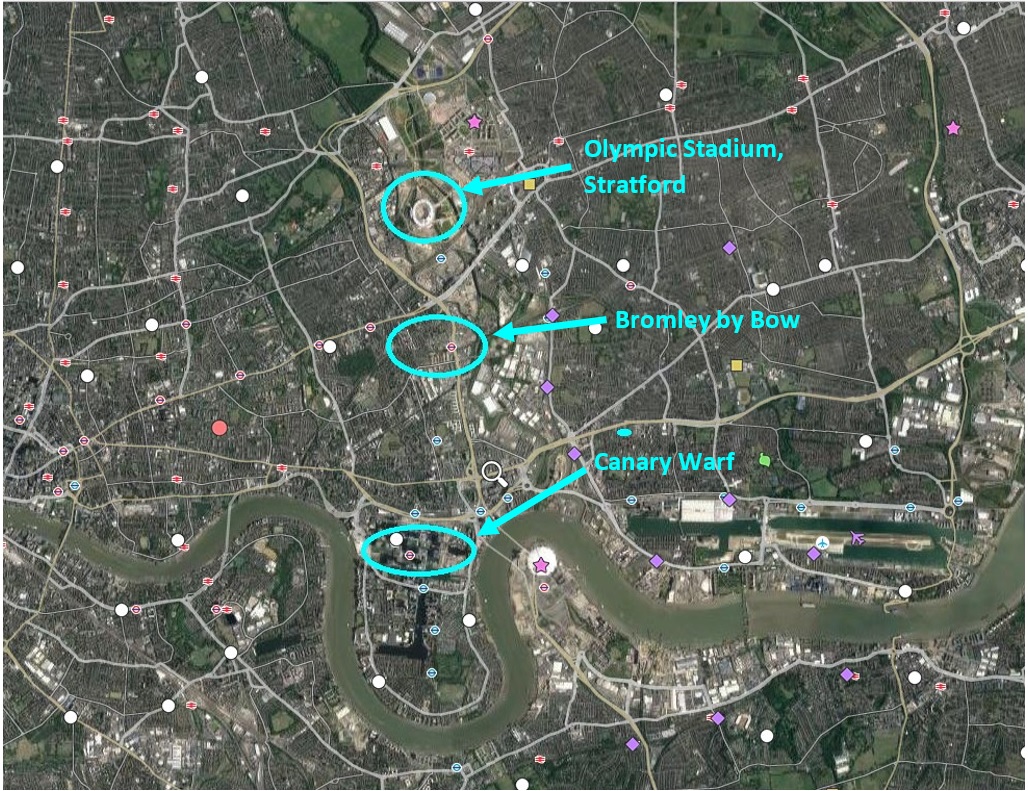
Edited image by Rebecca Jackson map via Google Earth
Effect of social determinants on health
In the 1890s Charles Booth created a map of London which categorized areas of the city of London depending on their levels of deprivation. The most recent Indices of Multiple Deprivation Report showed that those same areas considered deprived in the1890s are still facing the highest levels of multiple social deprivation and health inequality today. It is no secret that disadvantage has a negative impact on people’s ability to make the best choices when it comes to health. And disadvantage at a social level can have a significant influence on poor physical and mental health across a range of conditions.
More recent research conducted by Michael Marmot looked more closely at what determines health outcomes in populations, and the extent to which other factors influence people’s health, or rather their ability to be well.
He produced what is known as the 30/70 model: 30% of what determines your health is your genetics and improvements in pharmacology, the other 70% is related to other “external factors” including poverty, environment, culture, employment and housing. BBBHP has used this as the foundation for their primary care model, arguing that primary care providers are not just dispensers of medical products, but have a responsibility to contribute to people living healthier lives in their community.
Social prescribing
One issue highlighted by the BBBHP was the significant number of people presenting at GP surgeries with “non-medical” ailments, or medical ailments triggered by “non-medical stimulus”. People were arriving at the practices and booking appointments because they were lonely and it gave them somewhere to go. Others were presenting with symptoms of depression, which on further investigation were found to have stemmed from issues around debt or domestic violence. A social prescribing service was set up by the partnership to try to tackle some of these non-medical conditions and improve the health of the general population by non-pharmacological means.
The social prescribing service, where GPs refer people to other local services for help, can be used as a replacement for pharmaceutical interventions, or be supplementary to them. GPs, or other primary care staff, may refer any adults over the age of 18 to one of over 40 partnership organisations. These range from walking groups to formal sessions with advisors in debt or domestic violence agencies, as well as art classes, community gardens and companionship services to combat loneliness. The organisations can provide help and advice on issues such as employment and training, emotional well being and mental health.
The challenges of quality and funding
Maintaining quality in the provision of social prescribing is a particular challenge for BBBHP. They work regularly with trusted partners, particularly the Bromley by Bow Centre. However, there is no consistent quality check for many of the services from the health partners themselves. Evaluative studies and feedback sessions are used to assess quality and impact, and consider the scale of demand. And while it is acknowledged that more formal frameworks for assessing quality and impact of social prescribing services are preferred in formal assessments, in reality, word of mouth, participant feedback and uptake rates are used as a standard for quality as much as official feedback in a localised community setting.
A second issue is funding. BBBHP identified that finding long term funding was their main issue in providing security for providers and service users, as well as for GPs referring to services. Funding is vital not only to ensure the survival of the community groups who provide some of the referred services, but also to allow them to develop longer term partnerships and build capacity within the social prescribing service. The BBBHP works closely with the Bromley by Bow Centre, a key provider of support services for the local community, but like many services which rely on funding, they increasingly have to plan for tighter budgets.
A final challenge for the staff at BBBHP was changing people’s expectations of primary care, and what it means to live well. Some patients were suspicious and reluctant to be recipients of “social prescription”, as this did not fit with the traditional expectation of what GPs should do to make people well. This can be a big change in mindset for some people, according to Ian Jackson, when people come expecting to be prescribed antidepressants but are instead “prescribed” a walking club or a debt advice service. He noted that the reaction from patients can sometimes be confused or hostile, and some patients do not even turn up for referrals.
Improving patients’ understanding of the benefits of social prescription, ensuring people attend referral appointments, and that social prescriptions have a long term impact is something which BBBHP are hoping to research further. They feel that looking at the long term impact of non-pharmaceutical interventions and how these feed back into the wider agenda of tackling inequalities is important to allow the partnership to continue to build healthy communities and save on primary care costs in the long term.
Creating positive social connections to improve community health
Social prescribing and other associated projects have sparked new social connections. Members of the community have come together to form their own support groups. The Children’s Eczema support group run by local GPs and the DIY health scheme, which sought to educate and support parents who were anxious about minor ailments in children, have helped parents in the area to set up WhatsApp groups, organise coffee mornings and go to one another for support. Such initiatives are regarded by BBBHP as important in tackling wider, systemic social inequality in the area.
Currently, primary health care in communities is focused on illness. This needs to change, according to BBBHP, with local community-based health delivery based as much around social health as biomedical issues. Through its social prescribing and other services BBBHP has aimed to focus on supporting people in a holistic way, tackling health inequalities as well as biomedical illness, to allow them to make good choices to improve their health.
If you’ve enjoyed this article, you might also like more of our blogs on health and wellbeing:
Share
Related Posts
By Donna Gardiner While free school meals (FSM) have been available in England on a means-tested basis since 1944, recent years have seen a renewed focus upon the potential benefits of providing free school meals to all school-aged children. Currently, ....
Today sees the start of Community Garden Week 2023. Across the UK, communities will be celebrating the many and varied types of community gardens, from children’s and neighbourhood gardens to therapy gardens and allotments. The benefits of community gardens are ....
By Hollie Wilson At the start of 2020, an independent review was published setting out what needed to be done to bring about changes to the care system for children and young people in Scotland. At the heart of the ....
The “No Wrong Door” (NWD) programme means exactly that – there is no wrong door to turn to for young people seeking support. NWD works on several core principles, which include working with young people’s birth family or guardians, allowing ....